About us
The National Reye's Syndrome Foundation of the United Kingdom, now part of the RCPCH, was formed to provide funds for research into the cause, treatment, care and prevention of Reye's syndrome and Reye-like disorders, to inform both the public and medical communities and to provide support for parents whose children have suffered from these diseases.
About
This website contains content originally generated by the National Reye’s Syndrome Foundation (NRSF).
The Royal College of Paediatrics and Child Health (RCPCH) took over the work of the NRSF in 2012 and has been responsible for updating this content since. The founders and trustees of the NRSF have retained, and will continue to retain, an active involvement in guiding RCPCH’s work in this field.
History
The National Reye’s Syndrome Foundation was founded because there was a need in the UK for research into Reye’s syndrome – principally a children’s disease that affects the liver and brain.
The Charity was constituted by a Deed of Trust dated 10 August 1983 (Registered Charity No. 288064) with the object of providing funds for research into the cause, treatment, cure and prevention of Reye’s syndrome and Reye-like illnesses, to inform both the public and medical communities and to provide support for parents whose children have suffered from these diseases.
The Foundation has endeavoured to make the general public aware of the disease and the need for early diagnosis. The Foundation also provides support for parents whose children have suffered from Reye’s syndrome.
Trustees who served the Board of Trustees
The undermentioned served the Board of Trustees in the following capacity.
Chair:
- Mr Clifford S. Harrington MBE, CEng, MIMechE, MIEE (1983-2005)*
- Mr Julian R.R. Ebsworth MA(Cantab) (2005–2012)*
* throughout his term of office, as Chairman
Trustee members of the Board:
- Mrs Audrey Harrington (1983-1988)*
- Mr Amin M. Abdulla (1983-1993)**
- Mr Abdul Sattar FCA (1983-2000)
- Prof Alex P. Mowat MB. ChB, FRCP, DCH (deceased) (1984–1995)
- Mr Gordon H. Denney, FCA, Hon.FRCPCH (1986–2012)***
- Mrs Gillian M. Denney (deceased) (1989–1999)
- Mr R. David Fulford (deceased) (1993-2008)
Mr Ian Brown BSc (1993-2012) - Dr Susan M. Hall, BSc, MSc, MB BS, FFPH, FRCP(UK), Hon.FRCPCH (1995-2004)
- Dr John F.T. Glasgow, BSc, MD, DCH, FRCP(Ire), FRCPCH (2004-2012)
Hon. Secretary:
- Mrs Audrey Harrington (1983-1988)
Hon. Treasurer:
- Mr Amin M. Abdulla (1983-1986)
- Mr Gordon H. Denney FCA (1986-1989)
Hon. Administrator & Treasurer:
- Mr Gordon H. Denney FCA, Hon.FRCPCH (1989-2012)
Members who served the Medical and Scientific Advisory Board
Chair:
- Prof Alex P. Mowat, MB, ChB, FRCP, DCH (deceased) (1984–1995)*
- Dr Susan M. Hall, BSc, MSc, MB BS, FFPH, FRCP(UK), Hon.FRCPCH (1995-2004)**
- Dr John F.T. Glasgow BSc, MD, DCH, FRCP (Ire), FRCPCH) (2004–2012)**
* throughout his term of office, as Chairman
** as member of the Board – see below
Members:
- Dr Martin H. Bellman, MD, DCH, FRCP(UK), FRCPCH (1984–2012)
- Prof Barbara H. Billing, PhD, FRCPath (1984–1991)
- Prof Dame Barbara E. Clayton, DBE, MD, PhD, FRCP(UK), FRCP(Ire), FRCP(Edin),FRC(Path), FMedSci, Hon.FRCPCH, Hon.DSc, Hon.FIBiol (deceased) (1984–2011)
- Prof Frank A Fairweather. QHP, BSc, MB BS FRCPath, FIBiol, FFOM(Hon), MB (1984–2012)
- Dr John F.T. Glasgow, BSc, MD, DCH, FRCP(Ire), FRCPCH (1984–2004)
- Dr Susan M. Hall, BSc, MSc, MB BS, FFPH, FRCP(UK), Hon.FRCPCH (1984-1995: 2004-2012)
- Dr Victor F. Larcher, BA,MB, BChir, MRCP (1984–1991)
- Dr Marguerite S. Pereira, MD (deceased) (1984–1988)
- Dr Geoffrey Smerdon, MRCGP (1988–1991)
- Prof Sir Albert Aynsley-Green, MA,DPhil, MB BS FRCP(Edin), Hon.FRCPCH (1993–2012)
- Mr Charles Pascall, FRCS (1993-2012)
- Dr Jim R. Bonham, BSc, MSc, PhD, FRCPath (1996–2012)
- Dr Colin Kennedy, MD, FRCP(UK), FRCPCH (1996–2012)
- Emeritus Prof M. Stuart Tanner, CBE,MSc, MB BS, FRCP(Glas), FRCP(Lon). FRCPCH (1996–2012)
- Dr Michael P. Champion, BSc, MB BS, FRCPCH (2002-2012)
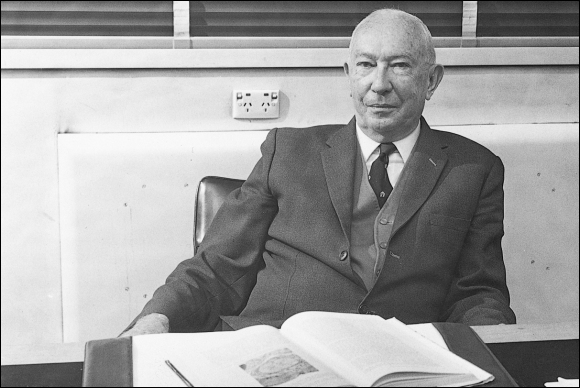
Douglas Reye (pictured below) was the first to describe the childhood disease now known as Reye Syndrome, and to recognise it as a distinct illness.
The causes of Reye Syndrome are still not known but it predominantly affects children between the ages of four and 16. According to the National Reye’s Syndrome Foundation, the disease “affects all organs of the body, but most lethally the liver and the brain. Reye’s Syndrome is a two-phase illness because it is almost always associated with a previous viral infection, such as influenza, cold, or chicken pox”.1
Douglas’s publication in The Lancet was the first description of the disease as a distinct syndrome. Equally important were Douglas’ observations on the histopathology of congenital rubella contained in Sir Norman Gregg’s original 1941 description of this syndrome, and his later identification in the 1960s of renal and other arterial stenoses in affected children.
Douglas was born in Townsville, Queensland in 1912. He moved to Sydney to study medicine at the University of Sydney, living at St Paul’s College until he graduated in 1937. He completed his Residency at the Royal Alexandra Hospital for Children where he remained for the whole of his active life. Although he enlisted in the army in 1940, there was a shortage of pathologists at the time and his release was obtained by the Hospital. He remained on the reserve for the length of the war.
Douglas was appointed acting-Director of the Department of Pathology at the Hospital in 1941 and became full-time Director in 1946. During his time has Director, Douglas expanded the Institute of Pathology to include “establishments for a microbiologist, biochemist and haematologist, fields which previously he had encompassed himself”.1
Douglas Reye was awarded a Doctor of Medicine in 1945 and worked for many years as a part-time Lecturer in Pathology at the University of Sydney.
Of his written contributions, J M Alexander writes:
“His bibliography was not voluminous but all publications dealt with entities which had either never been described previously or concerning which little had been written. His MD thesis concerned histiocytic reticulosis (one of his pet aversions was the term histiocytosis-X). He was the first to describe the subdermal fibrous tumours of infancy often referred to as Reteoma-1 and Reyoma-2. His main claim to fame worldwide was his description in The Lancet in 1963 of “Encephalopathy and fatty degeneration of the viscera: a disease entity in childhood” which has ever since been recognised as the Reye Syndrome.” 1
Alexander describes Douglas:
“Douglas was essentially a shy man and gave the impression of aloofness to those who did not know him well. Registrars and residents tended not to approach him but when forced to do so by those who knew him well, found that he was only too keen to share his great knowledge and experience with them.”
Douglas Reye passed away in 1977, two days after he retired.
There was a dramatic decline in classic aspirin-associated Reye’s syndrome after warning labelling on aspirin was introduced in 1986, and subsequently revised in 2003. This is largely due to the work of the Foundation’s medical and scientific advisory board which has earned the sincere thanks of parents and the general public. There have been no reported cases of classical Reye’s syndrome in the United Kingdom since April 2002.
In the 1980s the Foundation produced leaflets “Your child and Reye’s Syndrome – the facts the “dangers” and “After Reye’s Syndrome” designed to educate and inform parents, the public and professional bodies. The Foundation also produced a poster, which was circulated to all hospital paediatric departments throughout the country.
In the 1990s the Foundation funded studies into the pathogenesis of Reye’s syndrome and a pilot study into Medium-chain acyl-CoA dehydrogenase deficiency (MCADD – a Reye-like illness). Additionally the Foundation undertook the funding of surveillance of classical Reye’s syndrome from 1998 to 2000 following a decision by the Public Health Laboratory Service to curtail funding.
In March 2002 the Foundation funded a workshop at which invited experts considered various aspects of Reye’s syndrome and Reye-like illnesses. The main recommendation which emerged from the discussion: that a proposal was needed to develop a formal evidence-based guideline on the diagnosis and management of disordered consciousness.
A project to undertake this was subsequently begun at Nottingham in November 2003 under the direction of Professor Stephenson and funded by the Foundation. In 2005 this resulted in the publication of an evidence-based guideline by the Paediatric Accident and Emergency Research Group in Nottingham – “Management of a Child (aged 0 to 18 years) with a Decreased Conscious Level”. The guideline was disseminated to all members of the RCPCH.
The Foundation subsequently funded the RCPCH “Decreased Conscious Level multi-site audit” in 2010 and 2011; also the 2015 revised guideline – “The management of children and young people with an acute decrease in conscious level – a nationally developed evidence-based guideline for practitioners”. This guideline is in use in whole or in part in many children’s units.
Trustee reports
No trustee reports were prepared between 2010 and 2012; information was gathered which was to form the content of the redesigned website at that time and discussions were held with the RCPCH, which culminated in the handover in 2012.
Historical statement on the origin of the Foundation (45.7KB pdf) Trustees report - extracts 1986 (84.5KB pdf) Trustees report - extracts 1987 (21.3KB pdf) Trustees report - extracts 1988 (10.1KB pdf) Trustees report - extracts 1989 (27.3KB pdf) Trustees report - extracts 1990 (18.7KB pdf) Trustees report - extracts 1991 (17.9KB pdf) Trustees report - extracts 1992 (24.7KB pdf) Trustees report - extracts 1993 (28.4KB pdf) Trustees report - extracts 1994 (33.8KB pdf) Trustees report - extracts 1995 (41.4KB pdf) Trustees report - extracts 1996 (41.4KB pdf) Trustees report - extracts 1997 (61.5KB pdf) Trustees report - extracts 1998 (61.9KB pdf) Trustees report - extracts 1999 (60.0KB pdf) Trustees report - extracts 2000 (61.5KB pdf) Trustees report - extracts 2001 (58.1KB pdf) Trustees report - extracts 2002 (30.0KB pdf) Trustees report - extracts 2003 (38.8KB pdf) Trustees report - extracts 2004 (29.5KB pdf) Trustees report - extracts 2005 (34.6KB pdf) Trustees report - extracts 2006 (29.0KB pdf) Trustees report - extracts 2007 (18.1KB pdf) Trustees report - extracts 2008 (16.0KB pdf) Trustees report - extracts 2009 (19.1KB pdf) Advisory committee report - October 2013 (155.0KB pdf)Research
The total funds expended, and committed by the Foundation to research currently totals £696,364. This expenditure embraces the cost of studies into various aspects of Reye’s syndrome, contributions towards the purchase of equipment, amounts expended on workshops, reports, surveillance; also the creation, audit and revision of an evidenced-based guideline.
The funding of the original guideline “Management of a Child with a Decreased Conscious Level” was a major undertaking for the Foundation, and was followed some years later by the funding of a multi-site audit. As a consequence a decision was taken in 2013 to revise the original guideline which was completed in 2015.
A brief summary of the research activity, undertaken over the space of thirty-six years, together with the cost of each project is set out below.
Following the death of their daughter Katie in October 1981 Audrey and Clifford Harrington, in their quest to ascertain the cause of their daughter’s death, were put in touch with the Public Health Laboratory Service (PHLS) Communicable Disease Surveillance Centre (CDSC) in London. CDSC had already begun a national surveillance scheme for Reye’s syndrome in 1981, in collaboration with the (then) British Paediatric Association (now the Royal College of Paediatrics and Child Health). This surveillance scheme was funded at the time by the PHLS. The Harrington’s wanted the PHLS to undertake an epidemiological study into aspirin and Reye’s syndrome, somewhat akin to that which had been conducted in the USA some years earlier. Most of the funds needed for this extensive epidemiological study were not received through the Foundation, apart from a contribution of £29,000 from a pharmaceutical company between 1986 and 1989 of which £21,812 was applied towards this study.
A number of studies were undertaken at the Queen’ University of Belfast viz:
- Earmarked for studies into Reye’s syndrome in Northern Ireland between 1987/88 at a cost of £17,099. Due to the extensive use of aspirin in the Province the number of reported cases was particularly high.
- Studies into the pathogenesis of Reye’s syndrome undertaken between 1989/92, principally for specialist technical assistance connected with the study of Reye’ s syndrome: cost £33,000.
- Enzymological studies into the aetiology of Reye’s syndrome including the role of aspirin between 1991 and 1997: cost £118,000.
Further information about the above studies can be found in the Trustees’ Reports for 1991 through to 1999. See the Reports section.
- 1987 – a study with reference to electron microscopic appearances of Reye’s syndrome – grant £500.
During the year (1993) the Foundation contributed towards the part-funding of a pilot study into Medium chain Acyl-CoA dehydrogenase deficiency (MCADD) – a Reye-like illness, which was undertaken at Birmingham Children’s Hospital. The cost to the Foundation amounted to £13,300 inclusive of the cost of an MCADD poster prepared for an SSIEM meeting.
Further information about the above study can be found in the Trustees’ Reports for 1993, 1994, 1995 and 1997. See the Reports section.
During 1994 the trustees agreed to the funding of a study – “Surveillance of Adult Reye’s syndrome” undertaken at the University of Sheffield – Sheffield Children’s Hospital – at a cost of £51,915.
Further information about the above study can be found in the Trustees’ Reports for 1994 through to 1999. See the Reports section.
In 1995 the Foundation received a letter from Dr. Michael Catchpole of the Public Health Laboratory Service stating that the Communicable Disease Surveillance Centre was withdrawing from the surveillance of paediatric Reye’s syndrome before the 31st March 1996.
Shortly afterwards the trustees received a letter from Dr Susan Hall giving reasons why it would be unwise to discontinue surveillance of a condition of significant public health importance.
The trustees agreed to fund the annual cost which amounted to £15,000.
The tables of Reye’s syndrome surveillance produced annually from 1981/82 through to 2000/01 are reproduced in the Trustees’ Reports (Appendix) – from 1986 onwards, headed “British Paediatric Surveillance Report” .See the Reports section.
This was a feasibility study, undertaken in the year 2000, of a surveillance scheme to monitor the effectiveness of tandem mass spectrometry screening for inherited metabolic disorders when initiated as a national programme – cost £8,700.
Further information about the above study can be found in the Trustees’ Report for the year 2000. See the Reports section.
By Dr Susan Hall
- 20 years epidemiological surveillance of Reye’s syndrome in the UK.
- implementation of permanent storage of Reye’s syndrome database.
- proceedings of Workshop on Reye’s syndrome and Reye-like Inherited Metabolic Disorders (see note 11 and the opening paragraphs of note 14 below).
Cost of the 3 reports – £11,600.
- 1986 – Purchase – Experimental Blood Ammonia Checkers – cost £1,075. (contribution received from Ashford Police).
- 1988 – Queen’s University of Belfast – grant towards Hewlett Packard Gas Chromatograph Mass Spectrometer – £35,300.
- 1986 – Conference – “Reye’s Syndrome and Medication” held at “The Royal Society” in London – cost £524.
- 2002 – Workshop – “Reye’s Syndrome and Inherited Metabolic Diseases held at “The Stables, Doncaster – cost £6,207.
Further information is given in the opening paragraphs of the Decreased conscious level guideline section below, and also in the Trustees’ Reports for 2002 through to 2005). See the Reports section.
- 1993 – “British Isles” – Report for 1990/91 – the first decade of Surveillance” – cost £1,110.
- 2002 – Reye’s syndrome and aspirin – lest we forget – cost £284.
- 1993 – Poster: “Consider Reye’s or Inborn Errors of Metabolism” – for distribution to children’s hospitals – cost £841.
About the decreased consciousness clinical guideline
The project briefly described below is an ongoing major project of the Foundation and currently falls into three categories:
- the creation of the original decreased conscious level guideline in 2005
- an audit of the original guideline undertaken some five years later in 2010-2011
- the creation of the revised guideline to incorporate suggestions for improvement and correct weaknesses exposed by the audit. This third section of the project commenced in November 2013 and was completed in February 2015.
See more below.
In March 2002 the Foundation funded a workshop at which invited experts considered various aspects of Reye’s syndrome and Reye-like illnesses. The main recommendation which emerged from the discussion – that a proposal was needed to develop a formal evidence-based guideline on the diagnosis and management of disordered consciousness.
The Executive Summary and full proceedings of the Workshop can be found below.
Further information can also be found in the Trustees’ Reports 2003 through to 2006. See the Reports section.
A project to create the original decreased conscious level guideline subsequently began at Nottingham under the direction of Professor Terence Stephenson and led by Research Fellow Dr Richard Bowker. The project was funded by the Foundation at a cost of £96,750.
The aim of the project was the production of a national guideline on the management of children with an altered conscious level. Reye’s syndrome and Reye-like illnesses often present with an altered conscious level, whether that be confusion, drowsiness or a deep coma. As Reye-like illnesses are rare (some more rare than others) many health professionals will not have seen such conditions and may not think to look for them. A guideline which gives advice on what tests to perform, and what treatments to start will improve the ability of doctors and nurses to manage altered consciousness in children, including Reye’s syndrome and Reye-like illnesses.
Producing a national clinical guideline is a major undertaking. Doctors and nurses who have managed clinical problems one way will not change their practice just because a new guideline has been published. The guideline has to be produced to very high standards for it to be accepted nationally. To produce a national clinical guideline to high standards many different professionals need to be involved to discuss the key clinical questions which need answers and guidance. The guidance which is given needs to be based on the best evidence from clinical trials and research. To find the evidence numerous journals and scientific papers need to be searched to help answer the key clinical questions. Once the evidence has been found a recommendation can be based on what the evidence suggests is the right thing to do. Often, there is no evidence available to answer each specific clinical question. At this point expert opinion is required to help agree on further recommendations which will help to bridge the gaps between the evidence-based recommendations. Here again this process has to be thorough and incorporate as many views as possible from differing specialities, so that these recommendations are acceptable to all those involved in managing children with altered conscious level.
The year 2005 witnessed the publication of the evidence-based guideline by the Paediatric Accident and Emergency Research Group in Nottingham – “Management of a Child with a Decreased Conscious Level – a nationally developed evidence-based guideline for hospital practitioners” with the aim of improving and standardising assessment, investigations and treatment.
The University of Nottingham owns the guideline document. The guidance comprises 76 clinical questions covering 21 broad areas which focus on assessment, investigations, tests and the treatment of the underlying conditions secondary to decreased consciousness.
A public open day was held in Nottingham in 2005 to increase public awareness as to the existence of the guideline – cost to the Foundation £446.
An external appraisal process of the guideline by the College took place. The RCPCH Quality of Practice Committee appraised the guideline which was subsequently endorsed by the College. A decision was taken in 2006 to send a copy of the guideline to every member.
In 2007 the proposal for a national audit of the management of children with reduced consciousness was prepared by individual members of the RCPCH which were commented upon by members of the Foundation’s Medical and Scientific Advisory Board. The outcome was the College agreed to request the Foundation for funds restricted to the scoping/development phase which was undertaken in 2008 at a cost of £10,000. This resulted in the College publishing in February 2009 a draft work in progress Scoping Report and Development Plan. However, in March 2009 at an internal meeting at the College, it was decided that a national audit would not be the best way forward. In order to test the efficacy of the guideline the College proposed that a more limited (as opposed to national) project should be undertaken. Eventually it was decided that a multi-site audit should be carried out.
The background which led to the decision to undertake a multi-site audit is set out in the Trustees’ reports for 2008 & 2009. See the Reports section.
As a result of this decision the College published in 2009 an amended “Outline Project Plan for a Multi-site Audit” which detailed the project aims, methodology, organisation, governance and communication strategy. The report anticipated that the project would take 18 months to complete at a cost estimated at £156,274
The report “Care of Children and Young People Presenting to Hospital with a Decreased Conscious Level (Decon) – Multi-site Audit 2010-2011” was published by the RCPCH in February 2012.
In the foreword to the report, Professor Terence Stephenson wrote:-
“Six years on, this guideline is still as relevant now as it was then. It is with this in mind that the Decreased Conscious Level Multi-site audit project was commenced in 2010, again funded by the National Reye’s Syndrome Foundation.
This report examines some of the key recommendations of the guideline and provides an insight into the current position of the management of these children in hospital settings across the UK pointing to areas of good practice but also deficiencies in care.
This report’s findings have immeasurable importance for the enhancement of the quality of care of these children receive from all health professionals when they first present to hospital.
Finally I would like to pay tribute to the very hard work of Stephanie Smith and Carla Long in bringing the report to fruition.”
The revision of the original guideline was considered necessary because a number of suggestions had been put forward for improving the guideline, including the provision of more focused inclusion criteria and the inclusion for example of other common causes of decreased conscious level such as post-ictal convulsions, alcohol intoxication and febrile seizures. Additionally the guideline was considered to be too long and simplification of the algorithm and the adoption of a user-friendly linear approach was needed. The respondents of the survey indicated that the most important means of promoting guideline use was a one page algorithm of the guideline’s content, quick reference summary of the guideline, the provision of education and training sessions and the guideline summarised as a poster.
The project commenced in November 2013 and once the search for evidence was underway it soon became apparent there had been an information explosion in recent years. The revised guideline entitled “Management of children and young people with an acute decrease in conscious level – a nationally developed evidence-based Guideline for practitioners” was launched at the RCPCH annual conference in 2015.
In the foreword the College President Dr Hilary Cass wrote –
“The historical content of this Guideline is of considerable interest and importance, since it represents a triumph of collaboration over more than a decade.
“A Guideline is only of value if it remains clinically relevant and promotes good practice, and with this in mind the National Reye’s Syndrome Foundation UK went on to fund a multi site Audit in 2010-2011, which examined some of the key recommendations of the Guideline and provided an insight into the management of children with a decreased conscious level, across the UK, highlighting areas of good practice but also deficiencies in care.
“Maintaining its commitment to this important area of practice, the National Reye’s Syndrome Foundation UK has since gone on to fund the creation of the updated Guideline to incorporate suggestions for improvement and correct weaknesses exposed by the audit. The update of the 2005 Guideline was considered necessary because a number of suggestions had been put forward for improving the Guideline including, for example, other common causes of decreased conscious level such as post-convulsive states, alcohol intoxication, and febrile seizures. Additionally the Guideline was considered to be too long and simplification of the algorithm and the adoption of a user-friendly linear approach were needed.
“In 2002, following the dramatic reduction in Reye’s syndrome and Reye-like illnesses, the National Reye’s Foundation UK held a workshop at which invited experts considered various aspects of Reye’s syndrome and Reye-like illnesses. The main recommendation which emerged was the need to develop a formal evidence-based Guideline on the diagnosis and management of decreased consciousness. The National Reye’s Syndrome Foundation UK recognised that whilst decreased consciousness is one of the common modes of presentation for children with Reye’s or Reye-like conditions, it is also the endpoint of a wide range of serious illnesses which require urgent diagnosis and treatment in order to avoid secondary neurological damage or death. The initial 2005 Guideline was funded by the National Reye’s Syndrome Foundation UK, produced by the University of Nottingham and subsequently endorsed by the RCPCH and sent to every College member.
“The funds and work of the National Reye’s Syndrome Foundation UK were incorporated into RCPCH in 2012, but the legacy of the charity is ongoing. The contribution of a relatively small charity to such an important clinical area is immeasurable, and I would like to thank the National Reye’s Syndrome Foundation UK on behalf of the many children who are alive today because of its work.”
The cost of the revised guideline amounted to £96,627.
By the time the third stage of the decreased conscious level guideline had been completed, the Foundation’s total contribution to the project amounted to £360,097.
Surveillance
Epidemiological surveillance has been defined by the World Health Organisation as the collection, analysis and dissemination of high quality data relevant to the understanding, prevention and control of medical conditions of public health importance so as to satisfy the needs of health care professionals, science, government, voluntary organisations and the public at large.
Surveillance of Reye’s syndrome began in August 1981 as a venture shared between the (then) British Paediatric Association and the Public Health Laboratory Service Communicable Disease Surveillance (CDSC). Responsibility for case ascertainment was transferred to the British Paediatric Surveillance Unit (BPSU) in June 1986. The administration of the scheme was transferred from CDSC to the Department of Paediatrics at Sheffield in 1995. It ceased in 2001. Since then the only routinely available source of information is the adverse drug reaction reporting scheme of the Medicines and Healthcare Regulatory Agency.
In 1984-85 a risk factor study mounted on the surveillance database, showed there is an association between Reye’s syndrome and aspirin taken or given for relief of the symptoms of the viral infection which precedes it.
Since 1986 there has been a requirement that products containing aspirin must carry warning labels which was extended to patient information leaflets from April 1998. The incidence of “classic” Reye’s syndrome dropped dramatically with the introduction of these warnings. The last reported case of “classic” Reye’s syndrome occurred in the UK in April 2002.
All of the fifteen reports of the BPSU covering the years 1986/1987 to 2000/2001 are reproduced as an Appendix, in each of the Trustees’ reports for those years. (These reports can be found above.) Please see the BPSU website for further information.
It is now recognised that a number of inherited metabolic disorders – most notably those affecting fat oxidation, amino acid metabolism and ureagenesis may present as a “Reye-like” illness, which is clinically and pathologically almost indistinguishable from Reye’s syndrome, although there are some differences including the age distribution. See further information in the Metabolic Disorders section.
On 13 March 1985 following the issue of a Press Statement by the Foundation, the disease Reye’s syndrome was the subject of a Parliamentary written answer. In July 1986 the problem the UK had been experiencing with the disease was the subject of a lengthy debate in the House of Commons. The written answer and the extract from Hansard are reproduced as an Appendix in the Trustees’ reports for 1985 and 1986 respectively, see above.
References
Mellor, Lise (2008) Reye, Ralph Douglas Kenneth. Faculty of Medicine Online Museum and Archive, University of Sydney.
An alternate version appears in: Mellor, L. 150 Years, 150 Firsts: The People of the Faculty of Medicine (2006) Sydney, Sydney University Press.